Sleep apnea and type 2 diabetes are both common conditions, especially among middle-aged individuals and those with a modern, sedentary lifestyle. It is noteworthy that these two conditions are closely related to each other. More and more studies indicate that sleep apnea may be a significant risk factor contributing to increased insulin resistance and the development of type 2 diabetes. Understanding this connection will help with early intervention, more effective treatment, and reducing serious complications for patients.
What Is Sleep Apnea ?
Sleep apnea is a serious sleep disorder that causes the patient to stop breathing and then breathe again continuously while sleeping, with the duration of the breath cessation lasting from a few seconds to several tens of seconds depending on its severity. This condition will disrupt sleep and reduce blood oxygen levels, which over time can lead to serious health issues such as high blood pressure, cardiovascular disease, diabetes, and even stroke.
There are up to 3 types of sleep apnea, differing in the causes of the apnea phenomenon, including Central sleep apnea (CSA), complex sleep apnea, and the most common, obstructive sleep apnea (OSA). But all three still pose significant risks leading to serious bodily conditions due to lack of oxygen in the blood and metabolic disorders.
The common symptoms of sleep apnea include loud snoring, frequently waking up in the middle of the night, gasping for breath or feeling suffocated, headaches upon waking, excessive daytime sleepiness, difficulty concentrating, and frequent irritability or discomfort. Sleep apnea is commonly observed in patients who are male, older, overweight, smokers, and frequently consume alcohol.
What Is Type 2 Diabetes?
Unlike type 1 diabetes, which is a rare autoimmune disease (accounting for only about 5–10% of diabetes cases), often starting in childhood due to the immune system attacking the beta cells of the pancreas, causing the body to stop producing insulin, there is currently no effective prevention method. Type 2 diabetes, on the other hand, can be prevented or its onset delayed through a healthy lifestyle such as maintaining a reasonable weight, eating scientifically, and exercising regularly. However, lifestyle is not the only factor that increases the risk of type 2 diabetes, as age and genetic factors also play an important role. Therefore, even if you live a healthy lifestyle, you should still have regular health check-ups if you belong to a high-risk group.
Common symptoms of type 2 diabetes include frequent urination, constant thirst, unexplained weight loss, fatigue, blurred vision, and slow-healing wounds. The disease is commonly found in people who are obese, sedentary, older, or have family members who have had diabetes.
The Link Between Sleep Apnea and Type 2 Diabetes
Sleep apnea, especially the obstructive sleep apnea (OSA), not only causes fatigue and reduces sleep quality but also directly contributes to an increased risk of developing type 2 diabetes. This connection is explained through various biological mechanisms:
Low blood oxygen levels and chronic sleep disorders increase insulin resistance.
Lack of oxygen in the blood and chronic sleep disorders caused by sleep apnea will increase insulin resistance, leading to type 2 diabetes. Specifically, when patients repeatedly stop breathing during sleep, the oxygen levels in their blood decrease in episodes, also known as intermittent hypoxia. This condition, accompanied by continuous disrupted sleep, causes the body to enter a state of chronic stress. From there, it causes hormonal and metabolic disorders. As a result, the body no longer responds effectively to insulin, a condition known as insulin resistance. When insulin resistance increases, glucose in the blood is not transported into cells for use, leading to blood sugar disorders and increasing the risk of type 2 diabetes.
Systemic inflammation causes Glucose metabolism disorder
Sleep apnea not only disrupts sleep but also triggers a systemic inflammatory response throughout the body, known as systemic inflammation. These inflammatory substances interfere with insulin’s ability to function, preventing cells from effectively absorbing glucose. Glucose is the main source of energy for the body, especially for the brain and muscles. After a meal, glucose is absorbed into the blood, and insulin helps transport glucose into the cells for use or storage. When the body still has insulin but the cells do not “open the door” to let glucose in, glucose begins to accumulate in the blood. This leads to high blood sugar levels. As a result, the process of sugar metabolism is disrupted, leading to increased blood sugar levels and a higher risk of developing type 2 diabetes.
Hormonal disorders during sleep affect the ability to control blood sugar levels.
Sleep apnea not only disrupts sleep but also disturbs the hormone secretion process, including substances that regulate the sensation of hunger, satiety, and blood sugar levels.
- Cortisol, also known as the stress hormone, often rises at night in people with sleep apnea. This causes blood sugar levels to rise abnormally, even without eating anything.
- Ghrelin is a hormone that increases the feeling of hunger. It causes patients to crave more food, especially sweets or starchy foods.
- Leptin (the hormone that creates the feeling of fullness) decreases, causing the body not to feel full, leading to overeating and weight gain.
This hormonal imbalance makes it more difficult to control blood sugar levels, increasing the risk of developing type 2 diabetes or worsening the condition if already present.
See more: The Vicious Cycle Between Sleep Apnea and Obesity
Diagnosis
Accurate diagnosis is essential for identifying and managing both Obstructive Sleep Apnea (OSA) and Type 2 Diabetes, as these conditions often remain silent in their early stages. Early detection not only helps prevent complications but also improves long-term health outcomes. Each condition requires specific clinical tests and assessments to confirm the diagnosis and guide treatment.
Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea is primarily diagnosed through a sleep study known as polysomnography. This overnight test is performed in a sleep clinic or at home with portable equipment. It records various physiological parameters while the patient is asleep.
- Breathing patterns and number of apnea events
- Blood oxygen levels
- Brain activity (EEG)
- Heart rate and body movements
- Sleep position and snoring sounds
From this data, physicians calculate the Apnea-Hypopnea Index (AHI) to determine the severity of the disorder.
Type 2 Diabetes
Type 2 Diabetes is diagnosed through blood tests that measure glucose levels and long-term blood sugar control. The key tests include:
Fasting Plasma Glucose (FPG): The patient fasts for at least 8 hours before the test. A fasting glucose level of 7.0 mmol/L (126 mg/dL) or higher may indicate diabetes.
Hemoglobin A1c (HbA1c): This test reflects average blood glucose levels over the past 2 to 3 months. An HbA1c level of 6.5% or higher is considered diagnostic for diabetes.
Oral Glucose Tolerance Test (OGTT): After consuming a 75g glucose drink, blood sugar is measured after 2 hours. A reading of 11.1 mmol/L (200 mg/dL) or more suggests diabetes.
Random Blood Glucose Test: If a randomly measured blood glucose level is 11.1 mmol/L (200 mg/dL) or higher, it may be a sign of diabetes. If the patient also has symptoms such as frequent urination, excessive thirst, or unexplained weight loss, a diagnosis of diabetes may be confirmed.
Treatment of Sleep Apnea and Type 2 Diabetes
Managing both Obstructive Sleep Apnea (OSA) and Type 2 Diabetes requires a comprehensive approach. This includes lifestyle changes, medical treatment, and, in some cases, therapeutic devices or procedures. Addressing both conditions simultaneously can significantly improve overall health outcomes.
For Sleep Apnea:
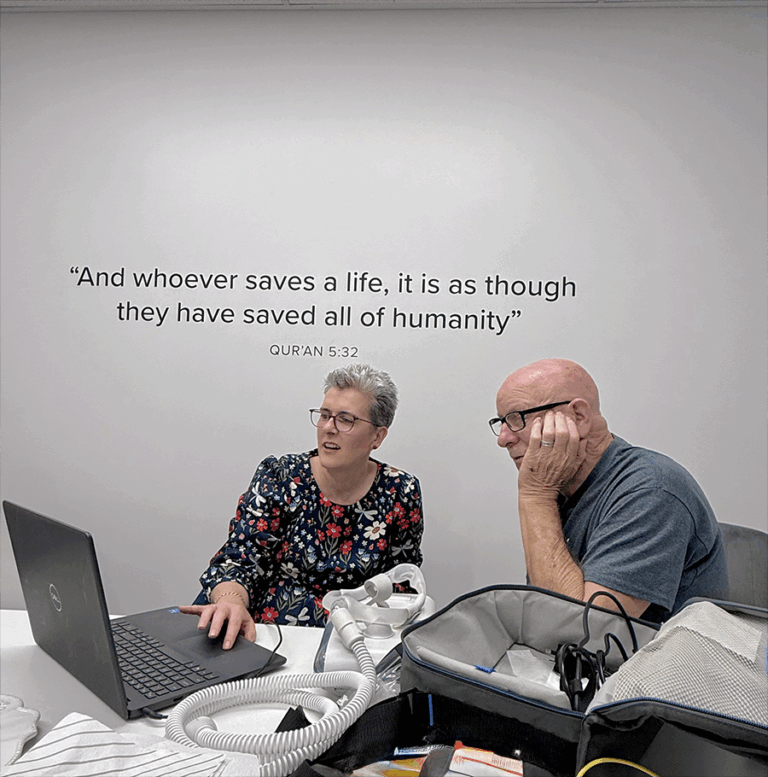
CPAP therapy (Continuous Positive Airway Pressure): This is the most effective and commonly used treatment. It delivers a constant stream of air through a mask to keep the airway open during sleep. This helps reduce apnea episodes and improve sleep quality.
Lifestyle modifications: Patients are advised to lose excess weight and avoid alcohol and sedatives, especially before bedtime. They should also try sleeping on their side instead of their back to help reduce airway obstruction.
Surgical intervention (if needed): In cases where anatomical issues contribute to airway blockage, surgical options such as UPPP or nasal surgeries may be considered. This is usually recommended when CPAP is not tolerated or proves ineffective.
For Type 2 Diabetes:
Healthy diet and physical activity: A balanced diet that controls carbohydrate intake, paired with regular exercise, is essential. These habits help manage blood sugar levels and improve insulin sensitivity.
Oral medications: Most patients begin with Metformin, a first-line medication that lowers glucose production in the liver and improves insulin response. Other medications may be added based on individual needs.
Insulin therapy (if needed): In more advanced stages, or when oral medications are not sufficient, insulin injections may be prescribed. This helps maintain proper blood glucose control.
Integrated Treatment Approach:
- CPAP therapy can help improve blood sugar control. By restoring oxygen levels and improving sleep quality, CPAP treatment can have a positive impact on metabolic health. It has been shown to reduce insulin resistance and stabilize blood glucose levels in patients with both OSA and Type 2 Diabetes.
- Better blood sugar control improves sleep. On the other hand, maintaining healthy glucose levels can reduce symptoms like nocturia (frequent urination at night), restlessness, and fatigue. This leads to better sleep quality and improved adherence to CPAP therapy.
Conclusion
Sleep apnea and type 2 diabetes are two common yet often overlooked health conditions that are closely interconnected. While each condition poses its own health risks, their coexistence can significantly amplify complications and reduce quality of life if left untreated. Fortunately, with timely diagnosis and appropriate treatments, both conditions can be effectively controlled. This includes CPAP therapy for sleep apnea, proper blood glucose management for diabetes, and healthy lifestyle changes.
Recognizing the link between poor sleep and impaired blood sugar regulation is a crucial step. It helps break the vicious cycle between these two diseases. For individuals living with either or both conditions, an integrated treatment plan offers the best chance of improving both sleep quality and metabolic health.
Reference
1. A Pandey, M Demede, F Zizi, et al. Sleep Apnea and Diabetes: Insights into Emerging Evidence. Current Diabetes Reports. 2011 Feb;11(1):35–40. doi: 10.1007/s11892-010-0164-9. PMCID: PMC4224959 NIHMSID: NIHMS562300 PMID: 21069483
2. Muraki I, Wada H, Tanigawa T. Sleep apnea and type 2 diabetes. Journal of Diabetes Investigation. 2018 Apr 14;9(5):991–997. doi: 10.1111/jdi.12823. PMCID: PMC6123041 PMID: 29453905