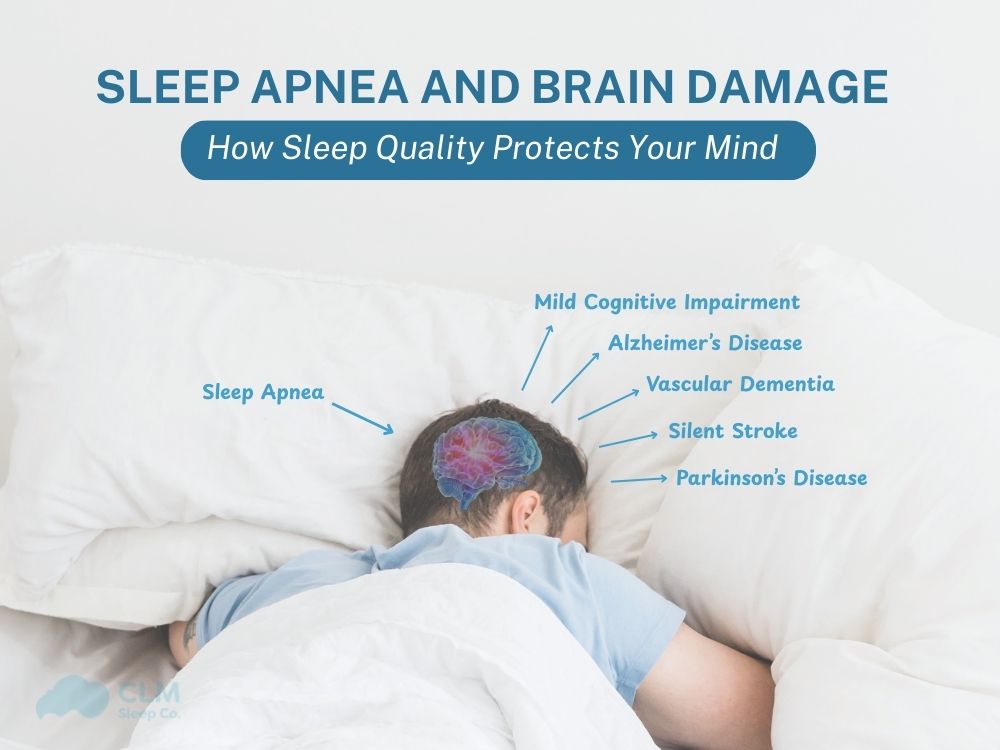
Sleep apnea and brain damage are a hot topic in modern sleep medicine. According to new studies, sleep disordered breathing not only affects sleep quality but also has the risk of causing profound damage to the brain. Especially for Australians interested in brain health, by understanding sleep apnea, health professionals have proven this connection to help people proactively prevent and protect brain function.
What is Sleep Apnea and How Does It Affect the Brain?
Sleep apnea is a breathing disorder during sleep, characterized by complete apnea or repeated hypopnea due to upper airway obstruction. The most common form is Obstructive Sleep Apnea (OSA). Characterized by the collapse of the throat and tongue muscles during sleep, narrowing or blocking the air circulation, leading to reduced or stopped oxygen supply to the body, and especially the brain.
Mechanisms of brain damage include:
- Prolonged hypoxia: When the brain is continuously deprived of oxygen, it causes oxidative stress, triggers an inflammatory response, and damages brain tissue.
- Nerve transmission imbalance: Symptoms of abnormal metabolism appear, affecting the process of transmitting information between nerve cells.
- Sleep apnea disrupts the deep sleep cycle: Patients often have symptoms of waking up many times, affecting sleep quality and the brain’s recovery period.
Areas of the brain that are vulnerable include:
- Hippocampus: Plays a key role in creating new memories, consolidating old memories and navigating in space.
- Frontal lobe: key area, mainly responsible for behavior, planning, problem solving and emotional control.
- Cerebral cortex: reception center, cognitive processing, language, ability to learn and adapt.
According to certified sleep coaches from CLM Sleep and medical research, continuous deep sleep is a crucial stage for the brain to recover. Only with enough deep sleep (90-120 minutes per night) can the brain repair small damages, regenerate neural connections and protect long-term cognitive function.
See more: How many hours of sleep do we need?
Can Sleep Apnea Cause Brain Damage?
The latest medical research has confirmed: sleep apnea and brain damage are closely related. MRI analysis shows that people with OSA have white matter hyperintensities, along with changes in the temporal lobe and hippocampus – directly related to memory and concentration.
- Research at the University of California, Irvine (May 2025) Hypoxia during REM sleep reduces the volume of the hippocampus and prefrontal cortex, thereby impairing memory function and concentration.
- A report published in the journal Neurology (June 2025) the severity of sleep apnea is directly related to the area of the brain damaged, even after accounting for the effects of age and blood pressure.
Symptoms and cognitive consequences
- Reduced short-term & long-term memory: Due to damage to the hippocampus, patients often forget what they have just experienced, reducing their ability to learn and remember long-term.
- Difficulty concentrating, reduced work/study efficiency: Damage to the frontal lobe and cerebral cortex makes the patient less concentrated, easily distracted, and slow to think.
- Impaired executive function: Decision making, problem solving, organizing and planning are all negatively affected by brain damage caused by sleep apnea.
Certified sleep coaches warn: Can sleep apnea cause permanent brain damage? If the disease is not detected, diagnosed, and treated promptly, this nerve damage can become persistent or long-lasting, increasing the risk of neurological diseases such as dementia, depression, and Alzheimer’s.
Is Brain Damage from Sleep Apnea Reversible?
Brain damage caused by sleep apnea was once considered permanent, especially with signs on MRI showing loss of brain white and gray matter volume. However, many recent medical studies have proven that specialized interventions from certified sleep coaches and the use of CPAP machines both provide a clear chance of recovery for the brain damaged by sleep apnea. The data all indicate:
- White matter damage: Almost complete recovery is possible after 12 months of CPAP treatment.
- Damage to gray matter/functional areas: Gradual improvement after 3–6 months, with treatment compliance.
- Improve cognitive symptoms: Better attention, reaction speed, and memory with improved quality and quantity of deep sleep.
Brain damage caused by sleep apnea is largely reversible if the patient adheres to CPAP treatment under the guidance of certified sleep coaches CLM Sleep. Recovery was highest in white matter, cognitive symptoms improved significantly each month. Early detection and ongoing treatment are key to optimal protection and recovery of brain function.
See more of the other serious effects of sleep apnea on the patient’s health: Sleep apnea and obesity, Sleep apnea and type 2 diabetes, Sleep apnea and heart disease
Neurological Effects of Sleep Apnea
Sleep apnea not only causes simple fatigue after each night but also creates silent, profound changes to the central nervous system. Medical research has confirmed that repeated hypoxia is the direct cause of brain cell damage and reduced neurotransmitter function. Detecting early signs can help patients be more proactive in protecting brain health.
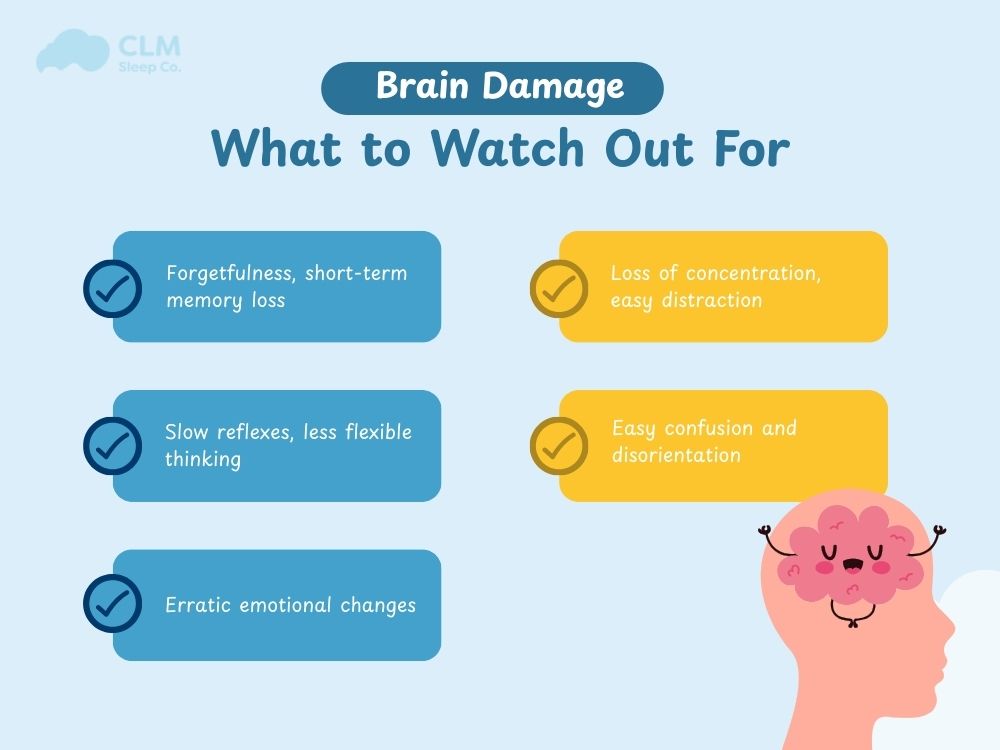
Early Warning Signs of Brain Damage
Sleep apnea causes many neurological consequences, which can be recognized through the following signs:
- Forgetfulness, short-term memory loss: Studies show that lack of oxygen during sleep causes the hippocampus to weaken. OSA patients often show signs of forgetting recent events, reduced ability to learn or remember information.
- Loss of concentration, easy distraction: Repeatedly low oxygen levels reduce brain circulation, affecting the prefrontal cortex. The consequence is reduced attention span and easy distraction when working or studying.
- Slow reflexes, less flexible thinking: White matter damage reduces the speed of signal transmission between brain regions. Patients find that reflexes are slower, thinking is no longer as sharp as before, and problem solving is poor.
- Easy confusion and disorientation: Damage to the frontal lobe and hippocampus causes difficulty in recognizing position and time, making it easy to get confused in everyday situations. This is an early sign of danger in adults and the elderly.
- Erratic emotional changes: Sleep apnea promotes chronic inflammation and changes the composition of neurotransmitter chemicals such as serotonin and dopamine. Patients are often irritable, sad, anxious or lose control of their emotions.
Common Neurological Disorders Related to Sleep Apnea
Sleep apnea increases the risk of neurological diseases such as:
| Neurological Disorders | Clinical Impact |
| Cognitive decline | Poor memory, attention, slow thinking |
| Dementia (Especially Alzheimer’s) | Accelerates the aging process, increasing the accumulation of amyloid plaques |
| Depression | Reduced interest, profound emotional changes |
| Anxiety disorder | Prolonged stress and anxiety reduce the ability to cope |
| Executive dysfunction | Reduced ability to plan and solve problems |
| ADHD/developmental delay in children | Difficulty concentrating, poor learning, slow formation of social skills |
Poor quality sleep directly impacts children’s ability to develop. Certified sleep coaches from CLM Sleep recommend early detection and intervention to prevent long-term consequences.
How to Safeguard Your Brain While Managing Sleep Apnea
Protecting brain function when managing sleep apnea requires a multi-pronged approach with the support of certified sleep coaches and modern medical solutions.
- Timely diagnosis: This helps prevent the formation of sleep apnea, helping to limit serious complications such as nerve damage, cardiovascular disease, high blood pressure and reduced cognitive ability.
- Using a CPAP machine regularly: helps maintain open airways, while also helping provide enough oxygen to the brain and minimizing the number of apneas each night while sleeping.
- Adjust your sleeping position and control your weight: Sleeping on your right side will help reduce the number of apneas and sleep apnea symptoms compared to sleeping on your back.
- Surgery, respiratory support devices: Applicable to cases of severe sleep apnea that do not respond to CPAP. Procedures such as UPPP, MMA or placement of oral appliances can significantly improve apnea index and sleep quality.
- Treatment of accompanying disorders: The rate of depression and anxiety in sleep apnea patients is very high. Simultaneous treatment of these disorders not only improves quality of life but also helps restore brain function more effectively.
Certified sleep coaches CLM Sleep will develop a personalized regimen, accompanying you every step of the way to improve your sleep health and protect your brain.

See more: Sleep Apnea Self-Care: Tips for Managing Your Condition
Conclusion
Sleep apnea and brain damage are health problems that cannot be subjective. The latest Australian studies show a real risk of brain damage if timely intervention is not performed. However, you can completely protect and restore your brain through in-depth diagnosis, proper treatment, combined with increasing the amount of deep sleep each night. Please proactively contact certified sleep coaches CLM Sleep to receive personalized advice. From there, build a deep sleep journey, improve brain function, and protect long-term health for you and your family.