Sleep and mental health have a two-way relationship, mutually affecting each other daily. Many studies have shown that adults need to sleep 7 to 9 hours each night to maintain physical and mental balance. When you don’t get enough sleep or can’t sleep deeply, the risk of encountering psychological issues such as stress, anxiety, and depression increases. Conversely, mental health conditions often disrupt sleep, leading to poor sleep quality, creating a vicious cycle that negatively impacts overall health and makes it more difficult for you to escape this condition. However, do you truly understand the nature of the relationship between sleep and mental health? Join CLM Sleep as we delve into the causes and how these two are connected
Read more: Why do we need sleep?
The Bidirectional Relationship Between Sleep and Mental Health
How Does Sleep Affect Mental Health?
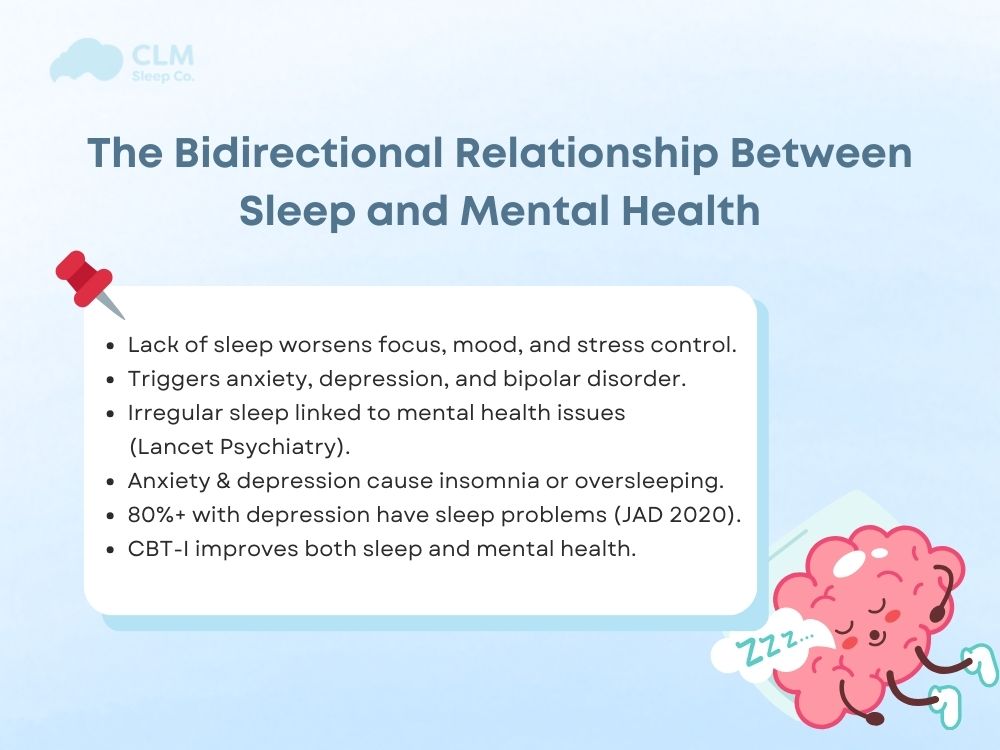
How does sleep deprivation affect mental health? Until now, the association between sleep and mental health has been well studied in scientific literature. Besides, being an impediment to cognition and emotional regulation, lack of eating can be an impediment to your psychological resilience. There are overwhelmingly many cases where lack of sleep serves as a primer for mood disorders such as anxiety, depression, and bipolar disorder.
A study published in The Lancet Psychiatry found people who suffer from insomnia or irregular sleep patterns are those prone to develop symptoms of depression and anxiety. A night of sleep loss can sometimes disturb both the sleep and mood, resulting in irritability, stress, and sadness the next day. On the other hand, a chronic lack of rejuvenating sleep can interfere with neurotransmitters and hormone activity, thereby aggravating an individual’s problems concerning mental health.
Additionally, you need to understand the stages of sleep. What is deep sleep? What is REM sleep? How do they affect your health?
How Does Mental Health Affect Sleep?
While sleep affects the mind, mental ailments can equally affect sleep. Attending to anxiety are those who often complain that racing thoughts or restlessness prevent them from falling asleep or staying asleep. The cycle of depression can lead to either hypersomnia (too much sleep) or insomnia (inability to sleep).
According to a 2020 study in the Journal of Affective Disorders, over 80% of individuals diagnosed with major depressive disorder also experience sleep disturbances. This bidirectional link between sleep and mental health suggests that improving one may positively influence the other. Cognitive Behavioral Therapy for Insomnia (CBT-I), for instance, is a proven treatment that not only helps with sleep but also reduces symptoms of depression and anxiety.
Sleep Apnea and Its Impact on Mental Health
Sleep apnea is a serious condition that goes beyond disrupted breathing. It plays a significant role in the complex relationship between sleep and mental health. While sleep deprivation is a major contributor to emotional and cognitive decline, it is not the only mechanism by which sleep apnea affects the brain and mood.
Repeated breathing interruptions during the night lead to fragmented and poor-quality sleep, causing persistent fatigue, difficulty concentrating, and emotional instability. Over time, this sleep loss can increase the risk of depression, anxiety, and mood swings. However, the impact does not stop at tiredness.
Sleep apnea also causes drops in blood oxygen levels, known as brain hypoxia. This lack of oxygen can damage neurons, impair memory, and reduce emotional resilience. In addition, people with sleep apnea often experience elevated activity in the sympathetic nervous system, which keeps the body in a constant state of stress – even during sleep.
Another important factor is hormonal imbalance. Disrupted sleep interferes with melatonin and cortisol production, both of which regulate mood and stress response. As a result, many patients report irritability, sadness, and a reduced ability to cope with daily stressors.
Addressing sleep apnea through medical treatment not only improves sleep quality but can also significantly enhance mental clarity, emotional stability, and overall sleep and mood.
Common Mental Health Issues Related to Sleep
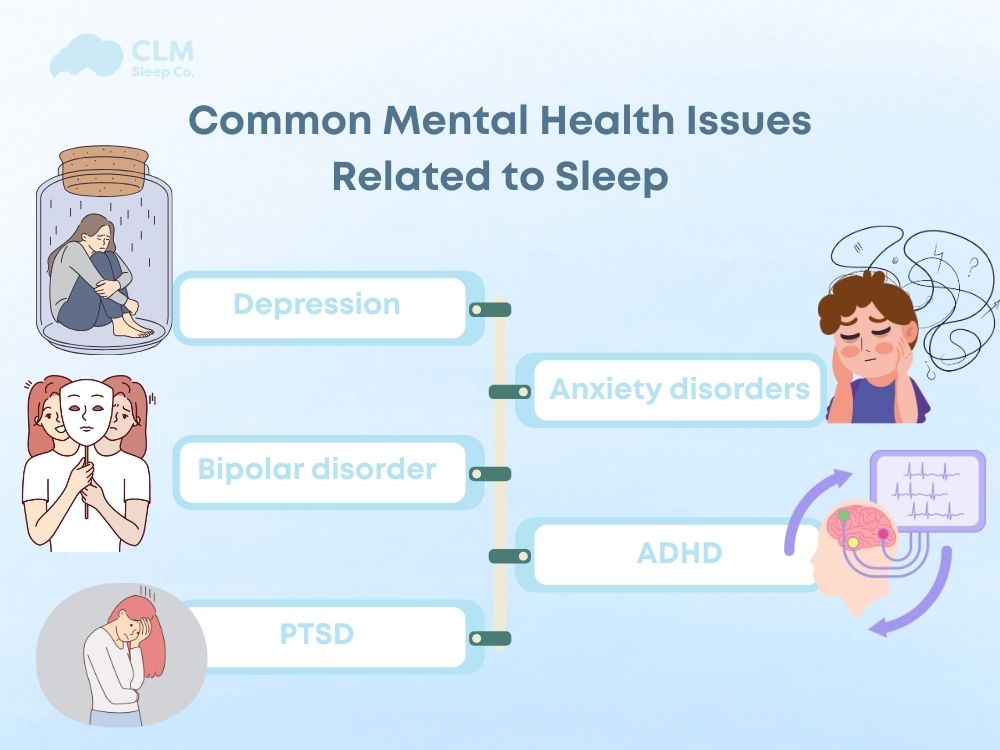
The relationship between sleep and mental health is deeply intertwined. Both poor sleep quality and disorders like sleep apnea or insomnia can contribute to the development and worsening of various psychological conditions. Sleep disruption not only affects mood and cognition but also increases emotional vulnerability and reduces the brain’s ability to recover from stress. Below are common mental health disorders strongly linked to sleep issues.
- Depression: Depression is closely connected to sleep disturbances. Many individuals with depression experience insomnia, early morning awakening, or excessive sleeping. Poor sleep can worsen low mood, reduce energy levels, and make it harder to concentrate. On the other hand, depression itself can interfere with the ability to fall or stay asleep. This creates a harmful cycle in which sleep and mood continue to decline together.
- Anxiety disorders: Sleep problems can intensify symptoms of anxiety. People who sleep poorly are more likely to feel nervous, overwhelmed, or unable to relax. Chronic sleep loss increases cortisol levels, which keeps the body in a state of alertness and stress. Over time, individuals with insomnia or disrupted sleep may develop generalized anxiety, panic attacks, or social anxiety disorders.
- Bipolar disorder: Irregular sleep patterns are a common feature in bipolar disorder. During manic episodes, individuals often sleep very little and feel unusually energetic, while depressive episodes are marked by oversleeping or extreme fatigue. Sleep apnea and frequent night awakenings can act as triggers, destabilizing mood cycles and making the condition harder to manage.
- ADHD or Attention Deficit Hyperactivity Disorder: People with ADHD often have trouble falling asleep, staying asleep, and waking up refreshed. Sleep deprivation can worsen symptoms like impulsivity, distractibility, and restlessness. In some cases, stimulant medications used to manage ADHD may also contribute to insomnia. Children and adults with ADHD are more likely to report fragmented or low-quality sleep, which affects learning and emotional control.
- PTSD or Post Traumatic Stress Disorder: Sleep disruption is a core symptom of PTSD. Individuals with PTSD frequently experience nightmares, flashbacks during sleep, or night sweats. These lead to fragmented rest and emotional exhaustion. Sleep disorders like sleep apnea may further reduce oxygen flow to the brain, intensifying symptoms such as irritability, mood swings, and hypervigilance. The long-term result is a reduced ability to process trauma and heal emotionally.
How Much Sleep Do You Really Need?
- Adults need between seven and nine hours of sleep each night
- Teenagers should aim for eight to ten hours
- Children require nine to thirteen hours, depending on their age
Consistency is essential. Going to bed and waking up at the same time every day helps regulate the body’s internal clock. This regular routine benefits both sleep quality and mental health.
Research shows that sleeping less than the recommended amount, and in some cases, significantly more, can increase the risk of mental health disorders and reduce overall well-being.
Read more: How Many Hours of Sleep Do We Really Need?
How to Improve Sleep and Strengthen Mental Health
Improving your sleep is one of the most effective ways to support emotional well-being. Quality rest enhances focus, reduces stress responses, and stabilizes mood. Here are key tips for better sleep:
For Everyone
- Keep a consistent sleep schedule: Go to bed and wake up at the same time daily, including weekends.
- Limit screens before bed: Avoid phones and laptops at least one hour before sleeping to reduce blue light exposure.
- Create a sleep-friendly environment: Keep your bedroom cool, quiet, and dark.
- Avoid stimulants at night: Limit caffeine and heavy meals before bedtime.
- Use relaxation techniques: Try meditation, light stretching, or deep breathing before sleep.
For People with Sleep Disorders
If you experience chronic sleep issues, early intervention is essential:
- Consult a specialist: Seek help if you have persistent insomnia, loud snoring, interrupted breathing, or constant fatigue.
- Follow a treatment plan: Conditions like sleep apnea may require CPAP therapy, oral devices, or lifestyle changes under medical care.
- Try cognitive behavioral therapy for insomnia (CBT-I): A proven, non-drug approach to treating chronic insomnia.
- Address mental health concerns: Conditions like anxiety, depression, or PTSD often disrupt sleep and should be treated by a professional.
- Use medication with caution: Only take sleep aids under medical supervision to avoid dependence.
Conclusion
Sleep and mental health are deeply connected. Poor sleep can worsen emotional health, while mental health challenges can disrupt sleep. By building healthy sleep habits and addressing sleep problems early, you not only improve rest but also support a more balanced, resilient mind. Prioritizing sleep is not just about feeling rested, it’s a vital step toward overall well-being.