Sleep apnea is a serious sleep disorder due to its widespread impact on cardiovascular health, metabolism, and daily quality of life. Early diagnosis and treatment are very important to prevent serious complications such as stroke or myocardial infarction.
Obstructive Sleep Apnea (OSA) is a disorder that, while often disregarded, has a major effect on the quality of life and longevity of millions of people worldwide. Imagine waking up after a night of “peaceful sleep,” only to find your body tired and your mind foggy , as if it had never actually rested. Obstructive […]
Central sleep apnea (CSA) is a rare type of sleep apnea, accounting for only about 5% of all cases. This disease is somewhat more complex and difficult to treat than OSA, because it involves the brain and nervous system. This condition can lead to fragmented sleep, reduced oxygen levels, and other health complications. Understanding the […]
Complex Sleep Apnea is a health issue that poses many risks, directly affecting the quality of sleep and the pulmonary and cardiac function of the patient. Recognizing and treating sleep apnea requires timely medical intervention, along with close monitoring. Therefore, to detect Complex Sleep Apnea early, you need to grasp the basic information about this […]
Do you have symptoms like loud snoring, waking up multiple times during the night, or feeling tired when you wake up? Don’t overlook these symptoms, as they could be signs of sleep apnea. With a home Sleep Apnea Test, you can easily and comfortably check your health right in your familiar surroundings. Let’s learn to […]
Apnea, meaning “stop breath,” refers to a temporary cessation of breathing. This condition can occur in various situations, from sleep disturbances to medical emergencies, and affects people of all ages, including infants. CLM Sleep will provide complete information about the different types of apnea, their causes, symptoms, potential complications, and available treatments to help you […]
If you get enough sleep but still feel tired, have difficulty concentrating or feel sleepy during the day. Then it is very likely that you are having sleep problems. This condition, if prolonged, will greatly affect the quality of life and lead to many health problems. A typical disease related to sleep disorders is sleep […]
Sleep apnea is a sleep disorder where breathing repeatedly stops and starts during sleep. This occurs due to a blockage in the airway (obstructive sleep apnea) or a failure in the brain’s signals to the muscles that control breathing (central sleep apnea). These interruptions can last from a few seconds to minutes and often result in loud snoring or choking sounds. Sleep apnea leads to poor sleep quality and can cause excessive daytime fatigue, making it important to recognize and treat this condition to improve overall health and well-being.
There are three common types of sleep apnea:
Obstructive sleep apnea (OSA) is the most common type and occurs when the muscles in the throat relax excessively, causing a temporary blockage of the airway. This blockage can disrupt normal breathing and lead to pauses in breathing during sleep. OSA is often characterized by loud snoring, choking, or gasping sounds. Risk factors include obesity, large tonsils, and a thick neck. It can result in fragmented sleep, excessive daytime drowsiness, and an increased risk of heart disease and high blood pressure.

Central sleep apnea (CSA) is less common and occurs when the brain fails to send the appropriate signals to the muscles that control breathing. Unlike OSA, there is no physical blockage of the airway. Instead, CSA is caused by a problem with the brain’s respiratory control center. This type of sleep apnea often affects individuals with underlying medical conditions such as heart failure or stroke. CSA can lead to irregular breathing patterns and periods of no breathing during sleep, causing disrupted sleep and daytime fatigue.

Complex sleep apnea (CompSA), also known as mixed sleep apnea, is a condition where both obstructive sleep apnea (OSA) and central sleep apnea (CSA) are present. Initially, a person may experience obstructive sleep apnea, characterized by physical blockages in the airway. However, after beginning treatment for OSA, central sleep apnea can sometimes emerge. This occurs when the brain fails to send the correct signals to the muscles responsible for breathing. Effective management of complex sleep apnea requires addressing both types of apneas simultaneously. This often involves adjusting treatment approaches, such as using specialized machines, and regular monitoring to ensure both obstructive and central breathing issues are properly managed.

The severity of sleep apnoea depends on how often your breathing is interrupted, usually measured by the Apnoea-Hypopnoea Index (AHI). As a guide:
Normal sleep
Fewer than 5 interruptions per hour (AHI < 5)
Mild sleep apnoea
Between 5 and 15 interruptions per hour (5 ≤ AHI ≤ 15)
Moderate sleep apnoea
Between 15 and 30 interruptions per hour (15 < AHI ≤ 30)
Severe sleep apnoea
More than 30 interruptions per hour (AHI > 30)
Symptom | Specific Manifestations |
Loud Snoring | Frequent, loud snoring is a common symptom, especially in obstructive sleep apnea. It may be accompanied by choking or gasping sounds. |
Excessive Daytime Sleepiness | Persistent drowsiness, fatigue, or the need to nap during the day despite having a full night’s sleep can indicate sleep apnea. |
Pauses in Breathing | Observed by a partner, these pauses can last for several seconds and are often followed by choking or gasping sounds. |
Restless Sleep | Frequent awakenings, restless tossing, or thrashing during sleep can be signs of disturbed sleep due to apnea. |
Morning Headaches | Waking up with headaches may be related to the poor sleep quality and oxygen deprivation associated with sleep apnea. |
Difficulty Concentrating | Problems with memory, concentration, and cognitive function can result from interrupted sleep and lack of restful sleep. |
Irritability and Mood Changes | Increased irritability, mood swings, or depression can occur due to chronic sleep disruption. |
Dry Mouth or Sore Throat | Waking up with a dry mouth or sore throat can be due to breathing through the mouth during sleep. |
What causes sleep apnea? The answer depends on the type. Below, we explore the main causes of the three most common forms of sleep apnea.


Complex sleep apnea occurs when a person initially has OSA, and treatment for OSA leads to the emergence of CSA. It involves a combination of both obstructive and central sleep apnea causes.

See more: Understanding Sleep Disordered Breathing
Several factors can increase the likelihood of developing sleep apnea. Understanding these risk factors can help in identifying individuals who may be more susceptible to the condition:
Obesity
Excess body weight, especially around the neck and abdomen, can increase the risk of sleep apnea. Fat deposits in these areas can obstruct the airway and contribute to breathing problems during sleep.
Gender
Men are more likely than women to develop sleep apnea, although the risk for women increases, particularly after menopause.
Alcohol and Sedatives
Consuming alcohol or using sedatives relaxes the muscles of the throat, increasing the likelihood of airway obstruction during sleep.
Posture
Sleeping on the back can exacerbate sleep apnea symptoms, as the position can lead to airway collapse or obstruction.
Gender Differences
Women may develop sleep apnea later in life, especially post-menopause, due to hormonal changes that affect the airway.
Ethnicity
Some studies suggest that certain ethnic groups may have a higher prevalence of sleep apnea compared to others.
Age
The risk of sleep apnea increases with age. This is partly due to changes in muscle tone and airway structure that occur as people get older.
Family History
A family history of sleep apnea or other sleep disorders can increase susceptibility, suggesting a genetic component to the condition.
Smoking
Smoking can increase inflammation and fluid retention in the upper airway, which can contribute to the development and worsening of sleep apnea.
Medical Conditions
Certain health conditions, such as high blood pressure, heart disease, stroke, diabetes, and hormonal disorders, are associated with an increased risk of sleep apnea.
Anatomical Features
Certain physical characteristics can contribute to sleep apnea, including a thick neck, a large tongue, enlarged tonsils or adenoids, a deviated septum, or a small upper airway.
Identifying and addressing these risk factors can help in the early detection and management of sleep apnea. If you have several of these risk factors and experience symptoms of sleep apnea, consulting a healthcare professional for evaluation and possible treatment is essential.
Screening for sleep apnea often involves using questionnaires to identify symptoms and risk factors. These questionnaires are valuable tools for clinicians to determine if further evaluation or diagnostic testing is necessary. Here are some commonly used questionnaires for screening sleep apnea:
Epworth Sleepiness Scale (ESS)
Measures daytime sleepiness and the likelihood of falling asleep in various situations. Consists of 8 questions about the likelihood of falling asleep during different activities, with responses rated from 0 (no chance) to 3 (high chance). A higher total score suggests greater daytime sleepiness, which may indicate sleep apnea or other sleep disorders.
Berlin Questionnaire
Assesses the risk of obstructive sleep apnea based on symptoms and risk factors. Divided into three sections: snoring, daytime sleepiness, and hypertension/body mass index (BMI). The answers help categorize individuals into high or low risk for sleep apnea.
STOP-BANG Questionnaire
Evaluates the risk of obstructive sleep apnea using a simple, effective tool. Consists of 8 questions that cover Snoring, Tiredness, Observed apnea, high blood Pressure (STOP), and Body Mass Index, Age, Neck circumference, Gender (BANG). A higher score indicates a higher risk of sleep apnea.
STOP Questionnaire
A shorter version of the STOP-BANG, focusing on the key risk factors for sleep apnea. Format: Includes 4 questions: Snoring, Tiredness, Observed apnea, and high blood Pressure. It helps identify individuals who may need further evaluation.
Pittsburgh Sleep Quality Index (PSQI)
Assesses sleep quality and disturbances over a one-month period. Includes 19 self-rated questions and 5 questions answered by a bed partner or roommate. It evaluates sleep quality, latency, duration, and disturbances. While not specific to sleep apnea, it helps identify overall sleep issues.
Sleep Apnea Clinical Score (SACS)
A clinical scoring system that combines multiple symptoms and risk factors to estimate the probability of sleep apnea. Includes questions related to sleep patterns, daytime sleepiness, and other relevant symptoms.
Modified Mallampati Score
Assesses the visibility of the throat structures to estimate the risk of airway obstruction. Involves an examination where the patient is asked to open their mouth and stick out their tongue. The visibility of the tonsils and soft palate is assessed to gauge airway obstruction risk.
These questionnaires are typically used in a clinical setting to screen for sleep apnea and determine if further diagnostic testing, such as polysomnography (sleep study), is needed. If you have symptoms of sleep apnea or are at high risk, these tools can help guide you and your healthcare provider in seeking appropriate diagnosis and treatment.
To accurately diagnose the severity and identify the exact type of sleep apnea, in addition to assessing clinical symptoms through questionnaires, patients need to undergo sleep studies. These tests provide concrete data that help determine the most appropriate and effective treatment plan. Below are some commonly used sleep study methods in Australia.
In-lab Polysomnography is the level 1 sleep study (which also includes Level 2 sleep apnea but is not widely used in Australia), highly accurate, conducted in a laboratory with the monitoring of sleep specialists. This method of sleep study is quite complex, involving the placement of about 15-20 sensors on the body and requiring overnight supervision and adjustment by sleep specialists. The measured indicators include:
Home sleep test (Level 3 sleep study) is a method of home sleep research that many Australians use due to its convenience and ease of implementation. This method uses about 4–7 sensors, which is somewhat simpler than a level 1 sleep study but still provides enough data to accurately diagnose sleep apnea. Level 3 sleep study measures the following indicators: Airflow, respiratory effort, oxygen saturation, heart rate.
Follow us at




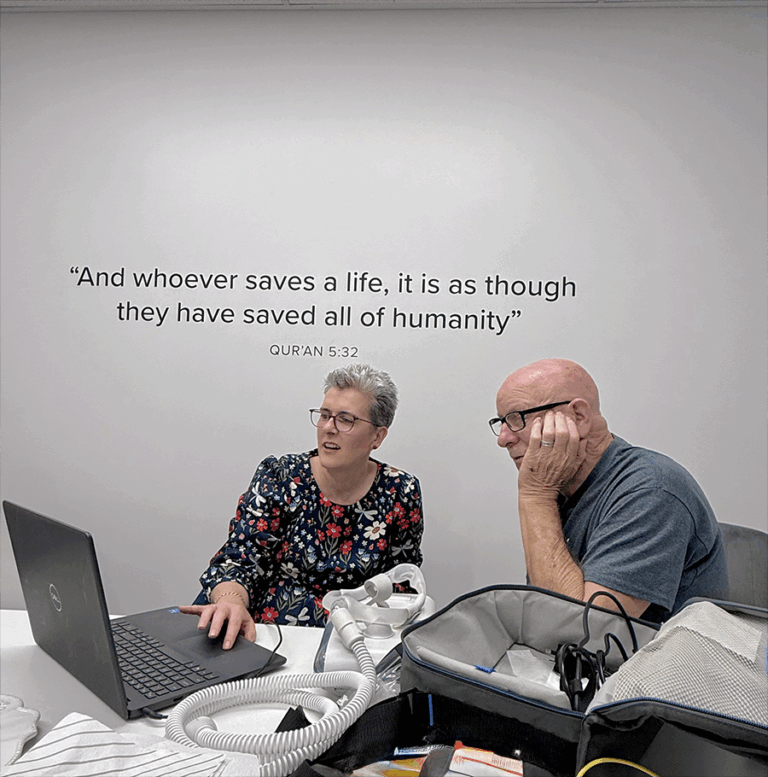
Lets take a moment to appreciate the beautiful art made by CLM Sleep Co. staff!


“CLM Sleep Co. gave me the patience, advice, and encouragement I needed to finally feel what better sleep is like.”
Patience Voice 2025




Nearly 20 stops, countless smiles, and one dream we all share — better sleep, every night.
CLM Sleep Co. is actively committed to promoting sleep-health awareness within the community, extending our efforts beyond workshops to educational settings. We collaborate with local schools, like Blackfriars Priory School in Prospect, South Australia, to deliver impactful presentations on the significance of sleep-health.
Our engaging sessions empower students with valuable insights, equipping them with essential knowledge to take control of their sleep routines and overall well-being. By fostering sleep literacy among the younger generation, we aim to sow the seeds of healthy sleep habits early on, ensuring a brighter and more rested future for our community.
April 03, 2024
Imagine a group filled with community spirit and yoga mats. That’s exactly what “Stretch for a Cause” was all about! Our community came together to stretch, breathe, and make a difference.
Led by a skilled instructor, we flowed through poses, feeling the positive vibes. But this wasn’t just any yoga class – it was yoga with a purpose. The funds we raised went straight to a charity close to our hearts.
“Stretch for a cause” was a blend of relaxation and giving back. We bent, twisted, and reached for a brighter future, one pose at a time. Thanks to everyone who joined in, making it more than just a yoga class, but a real force for good.
May 06, 2024
A safe, supportive Community on Facebook for Australians facing sleep issues like insomnia, sleep apnoea, or restless nights. Share experiences, ask questions, discover sleep tips, and connect with people
who truly understand what better sleep feels like.